Introduction: Despite the progress that has been made for standard risk multiple myeloma (MM), subsets of patients with the most advanced and aggressive plasma cell dyscrasias still suffer comparatively poor outcomes. One example is plasma cell leukemia (PCL), which carries a median overall survival of under two years. For patients with PCL, response to front line therapy occurs but is often short-lived, ultimately giving way to aggressive multi-drug resistant disease and patient mortality. Thus, there is a need for the development of new strategies that improve the prognoses for these patients. Melflufen (melphalan flufenamide) is a first-in-class peptide-drug conjugate that is currently in late-phase clinical trials for multiple myeloma. This highly lipophilic agent is preferentially retained in malignant plasma cells (MPCs), where overexpressed aminopeptidases lead to trapping of the alkylator melphalan. We evaluated the anti-myeloma effects of melflufen on patient samples treated ex vivo, and found pronounced sensitivity to melflufen in most samples, with particularly potent efficacy in PCL samples.
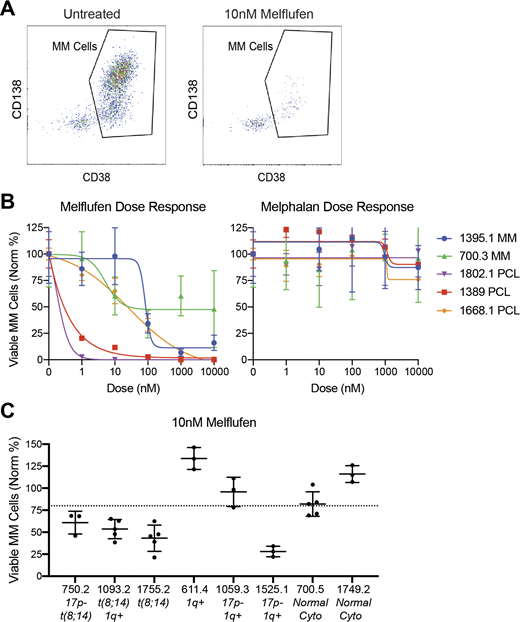
Methods: Bone marrow aspirate or peripheral blood samples were obtained from patients with plasma cell disorders after IRB approval and informed consent. Ex vivo efficacy of melflufen and melphalan were compared using our Myeloma Drug Sensitivity Testing (My-DST) platform that optimizes viability and tests the malignant cells in the context of the normal cells from their microenvironment (Walker et al, Blood Advances, 2020). In brief, mononuclear cells from patients with plasma cell dyscrasia, including MM and PCL, were isolated and cultured in triplicate wells with titrations of melphalan, melflufen or untreated controls for 48 hours. Post-treatment survival was measured by high-throughput flow cytometry with antibodies for CD138, CD38, CD45 and CD19, and a live/dead dye to discriminate viable MPCs from normal bone marrow cells. EC50 values were determined from these titrations using nonlinear regression curve fits. When the EC50 for melflufen was established in My-DST, a single dose concentration of 10 nM was used to screen patient samples and distinguish relative sensitivity or resistance.
Results: Using the My-DST approach with 48 hour drug treatments, melflufen significantly decreased the viable MPC populations, whereas melphalan had little effect (Fig 1A). Concurrent titrations revealed significantly higher MPC sensitivity to melfufen (mean melphalan EC50 = not reached, mean melflufen EC50 = 22.9 nM) (Fig 1B). By comparison to another alkylator, cyclophosphamide's active metabolite has an EC50 of 3.75 µM in this assay. Response to melflufen was accentuated in 2/3 PCL samples tested (HTB-1802.1, HTB-1389.1), with the EC50 < 1nM (Fig 1B). Melflufen demonstrated toxicity in CD45 positive white blood cells, which is consistent with neutropenia observed in clinical trials (data not shown). In single dose screening studies in additional MM patient samples, 4/8 (50%) showed >20% decrease in viable MPCs after incubation with melflufen at 10 nM (Fig 1C). Overall, using those parameters for ex vivo "response" to meflufen, 3/3 patients with PCL responded, 5/6 patients with del(17p) responded, and 3/3 patients with c-MYC translocations responded (Fig 1C, italics). In addition, 3/5 samples from patients that were clinically daratumumab-refractory displayed sensitivity to melflufen. Of five samples from patients with prior exposure to alkylators, four were sensitive to melflufen.
Conclusion: Overall, these data support that the peptide-drug-conjugate melflufen shows a broad efficacy across samples from patients with plasma cell disorders. Patients facing poor prognoses, including those with PCL, high-risk cytogenetics and daratumumab-refractory disease, have a great need for new treatments. Thus, the encouraging ex vivo results with melflufen in samples from these aggressive subsets support further clinical exploration. In particular, our preliminary data suggest that plasma cell leukemia patients may be exquisitely sensitive to melflufen. To follow-up these findings, we will expand the number of samples tested from PCL and other forms of high-risk MM samples. Ultimately, if the trend for accentuated sensitivity in plasma cell leukemia holds, a clinical approach for melflufen in these patients may improve outcomes for this group.
Lockerbie:Oncopeptides AB: Current Employment. Flanagan:Oncopeptides AB: Current Employment. Lehmann:Oncopeptides AB: Current Employment. Forsberg:Celgene: Speakers Bureau; Genentech, Inc., Sanofi, Karyopharm, Abbvie: Research Funding. Mark:Takeda: Consultancy; Kayopharm: Consultancy; Bristol-Myers Squibb: Research Funding; Janssen: Research Funding; Celgene: Consultancy; Amgen: Consultancy; Sanofi: Consultancy; Janssen: Consultancy. Sherbenou:Oncopeptides Inc.: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal